Minimally invasive spine surgery techniques have tremendously changed the way spine surgery is performed over the last couple of decades. Minimising the amount of muscle dissection as well as resection of bone, while achieving adequate decompression of the neural structures has been the constant endeavour of the minimally invasive spine surgeons.
The emergence of endoscopic disc surgery in the recent years is revolutionising the surgical treatment of degenerative spinal disorders, especially in lumbar spine. This has definitely made it possible to avoid a fusion surgery, involving stabilisation of spinal segments with implants, in certain situations.
For example, a patient with a recurrent disc prolapse at the same level after a prior laminectomy in the past may end up needing a fusion surgery by the conventional way of treatment. Also, a second conventional micro-discectomy through the scar tissue has higher risk of complications like dural tear, spinal fluid leakage or nerve root injury.
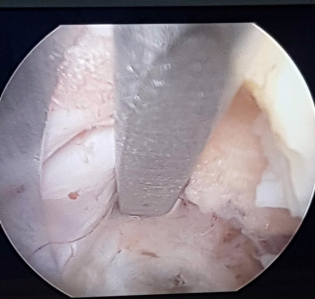
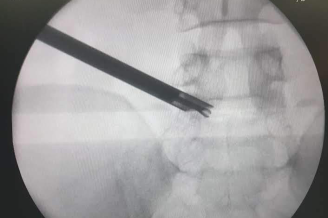
A transforaminal endoscopic discectomy provides the option to remove the prolapsed disc fragment through a different route, avoiding surgery through the scar tissue as well as the need to resect more bone, thereby preventing the need for a stabilisation and fusion.
Another example is a large central disc prolapse in upper lumbar segments or in a primarily narrow spinal canal. As the facet joints might need to be excised (to minimise the risk of neural injury) thereby making the segment unstable, a stabilisation with pedicle screws and fusion procedure is usually done in addition to the decompression.
But a transforaminal endoscopic discectomy can be performed without destabilising the segment and without increasing the risk of neural injury, thereby avoiding the need for a fusion surgery.
Patients with lumbar canal stenosis needing surgical decompression would many times need significant resection of the bone and facet joints to create adequate space for neural structures, making that segment unstable. Stabilisation with implants and fusion is an imperative part of the surgery in such situation. Endoscopic decompression of a stenotic spinal canal is now possible with the advanced instrumentation specially designed for stenosis, without destabilising the spinal segment, thereby avoiding the need for a stabilisation and fusion procedure.
Spinal stabilisation and fusion surgery has a definite role in management of lumbar degenerative disorders and is inevitable in some situations. But, with minimally invasive techniques and endoscopic spine surgery techniques evolving into reliable non-fusion options for most of the situations that need surgery, the need for a fusion procedure is becoming less frequent.
If you liked the article, please share it and subscribe to my future articles on spine problems. Thank you.!

With years of experience in spine surgery, Dr Phani Kiran S, Senior Consultant Spine Surgeon will assess you and suggest the treatment option that is right for you.
We at Medspine clinics, understand the importance of educating all our patients about the spinal problems and the most effective ways to take care of their spine.
The Ortho Clinic: Monday, Wednesday, Friday, Saturday.
Ojas Health: Tuesday, Thursday
© Copyright 2024 MedSpine. All Rights Reserved. Build with 🤍 by Digital GYB
WhatsApp us